The absence of residual disease after cytoreductive surgery (CRS) is the most important prognostic factor in the management of patients with advanced ovarian cancer (AOC). As a result, the therapeutic approach to these patients is based primarily on disease quantification to decide between neoadjuvant chemotherapy or cytoreductive surgery, so proper patient selection is critical because the complete cytoreductive surgery will depend on this fact.
The peritoneal cancer index (PCI) is a measurement of the volume and extent of peritoneal disease based on a description of the location and size of tumor implants by anatomical region [1]. PCI is an objective and reproducible tool for quantifying tumor burden in AOC patients [2].
The intraoperative PCI estimation is largely subjective; the pathological PCI differs significantly from the surgical PCI and can provide a more precise assessment of the extent of peritoneal cancer; thus, using the pathological PCI will allow for more objective comparisons between different studies [3].
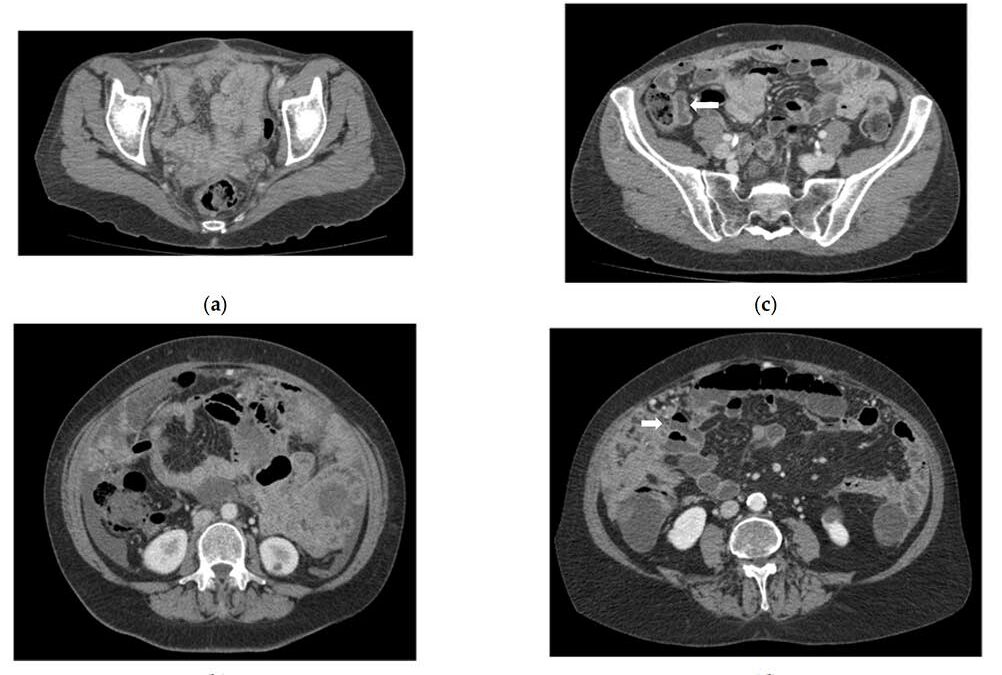
Multidetector computed tomography (MDCT) is the current imaging modality of choice for peritoneal carcinomatosis evaluation. Routine CT (rCT) is the usual technique to assess the extension studies of abdominal neoplasms, its main limitation is the inability to assess mesenteric involvement and small peritoneal deposits in the intestinal serosa [4]. A previous study identified CT enteroclysis (enteral contrast is introduced via a nasojejunal tube placed fluoroscopically prior to CT examination) as a reliable preoperative mapping of the extent and distribution of PC in the small bowel and mesentery [5]. According to another report, using CT enterography (where patients drink oral contrast) as a technical modification would improve the limitations of routine CT [6]. Enteral contrast is employed in both techniques to dilate the intestinal loops. However, enteroclysis requires the placement of a nasojejunal tube under fluoroscopic control, which increases radiation exposure and demands more ward and radiological time.
CT enterography (CTE) is a technique that combines intestinal distension resulting from the administration of a large volume of enteric contrast with the acquisition of sectional images after intravenous contrast administration.
The purpose of this study is to analyze the diagnostic accuracy of routine CT (rCT), CT Enterography (CTE) for the detection of lesions at the regional level (R0 to R8 and R9 to R12) compared with surgical and pathological reference standards, and to compare the agreement and diagnostic performance of routine CT (rCT), CT enterography (CTE) and surgical in PCI scoring with reference standards, in patients with tubo-ovarian peritoneal carcinomatosis.
More information: CT Enterography for Preoperative Evaluation of Peritoneal Carcinomatosis Index in Advanced Ovarian Cancer